Breast Reconstruction Thousand Oaks
Breast reconstruction encompasses a number of procedures that restore or recreate the breasts after treatment for breast cancer (e.g. mastectomy). There a variety of operations that can be divided into two basic categories: procedures that use your own tissue (borrowed from somewhere else on the body), or procedures that use only implants to restore the lost breast volume. Procedures that use your own tissue are termed “autogenous reconstruction.” The most common are the TRAM flap, the DIEP flap, and the latissimus flap.
Before & After Photos
 Breast Reconstruction
Breast Reconstruction
At the Kryger Institute of Plastic Surgery, we have experience in a vast array of surgical and non-surgical procedures. Click below to see some before and after photos of mommy makeovers.
MORE BREAST RECONSTRUCTION PHOTOS
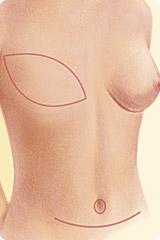 The TRAM and DIEP flaps leave scars similar to a tummy-tuck on the abdomen, and a scar on the breast where the nipple-areola and surrounding skin are removed during the mastectomy.
The TRAM and DIEP flaps leave scars similar to a tummy-tuck on the abdomen, and a scar on the breast where the nipple-areola and surrounding skin are removed during the mastectomy.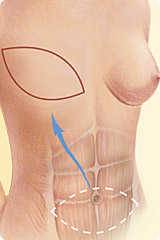
Skin (with or without underlying muscle) are transferred from abdomen to the chest in order to create a new breast.

An implant-expander reconstruction uses the same mastectomy incisions and leaves no new visible scars.

The latissimus flap procedure transfers skin and underlying muscle from the back to the chest wall in order to create a new breast.
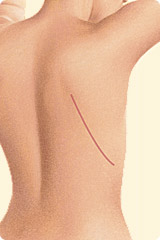 The latissimus flap procedure leaves a linear scar on the back where the skin was taken from.
The latissimus flap procedure leaves a linear scar on the back where the skin was taken from.What is microsurgery and how does it relate to breast reconstruction?
Microsurgery is a highly specialized field of plastic surgery. It involves the use of an operating microscope to perform the surgery. This is necessary in some breast reconstructive techniques when very small blood vessels have to be sewn together in order to create a new breast. These include several variations of the TRAM flap, the DIEP and SIEA flaps. Our surgeons are well-trained in microsurgery and have published articles and book chapters on the topic.
What is the TRAM flap breast reconstruction? What is the DIEP flap?
The TRAM flap involves creating a new breast using the excess skin, fat and rectus abdominus muscle from the abdomen. The traditional TRAM flap takes all of the muscle with it. A muscle-sparing TRAM takes only part of the rectus muscle leaving the rest in place. The DIEP is similar to the TRAM flap in that it also uses the extra tissue of the abdomen. It differs from the TRAM in that the rectus muscle is not taken. Hence the DIEP flap is composed only of skin and fat. The TRAM and DIEP flaps are generally used to reconstruct a breast after mastectomy. In some cases, they can also be used to restore a failed breast reconstruction.
Is the DIEP flap better than the TRAM flap?
This is a controversial topic in the field of breast reconstruction. The majority of scientific studies do not show a major difference between the two techniques. Although the TRAM flap is less technically challenging than the DIEP flap, the surgeons at the Kryger Institute are well-trained in both techniques and offer both procedures. Not all women are candidates for a DIEP flap. This can often only be determined at the time of surgery. For most women, there is not a noticeable difference between the two procedures in terms of results or complications. For women who are very athletic and do a lot of sit-ups, the DIEP flap may be a better choice.
What is the SIEA flap?
The SIEA flap is another autogenous flap from the abdomen. It is similar to the DIEP flap in that only skin and fat are taken to create a new breast. The advantage over the DIEP flap is that the entire flap can be harvested without having to cut into the abdominal muscles. Unfortunately, very few women have the special anatomy required to be candidates for an SIEA flap. This can only be determined at the time of surgery. Our surgeons have experience with the SIEA flap and will perform it in the appropriate patient.
What about the latissimus flap?
This reconstructive technique can be used after mastectomy or after lumpectomy (breast conservation therapy). It is also often used to reconstruct a breast that has a poor result from a previous implant reconstruction. This technique uses extra skin, fat and muscle from your back to create a new breast. Since there is usually not a lot of extra tissue on the back, an implant is often placed underneath the latissimus flap.
What does an implant/expander reconstruction involve?
An implant/expander reconstruction is performed after a mastectomy. This technique is usually a two-step process. The first stage involves placing a tissue expander underneath the pectoralis (chest) muscle. The expander is gradually inflated like a balloon by filling it with saline. This is done weekly in the office starting about 2-3 weeks after surgery. Once the skin has been adequately expanded, a second surgery is planned. The second stage involves removal of the expander and replacement with a permanent implant (either saline or silicone). The ideal candidate for this procedure is a woman who is thin-framed with small breasts, will have a mastectomy on both sides, and will not require radiation after surgery. Nevertheless, many women who do not meet all three of these criteria can still have a very nice result from an implant reconstruction.
How do I know what procedure is right for me?
At your initial consultation, your surgeon will discuss all the options with you. This will be a lengthy discussion lasting 30-60 minutes. It is our goal that no one leaves after a breast reconstruction consultation with doubts or unanswered questions. The procedure that you choose will be based on your desires and goals, lifestyle, overall health, and body type. In addition, previous breast surgery, a history of breast radiation and whether or not one or both breasts are being reconstructed all come into play. You can rest assured that all options will be discussed.
What about symmetry procedures on the other breast?
If you are only having cancer surgery on one breast, you may be a candidate for a procedure on the other breast in order to make it more closely match the reconstructed breast. These symmetry procedures include augmentation, reduction, or lifting of the breast. All breast reconstruction as well as symmetry procedures are covered by insurance as mandated by the Federal law.
Preparing for surgery
If the surgery is to be performed immediately following a mastectomy, coordination between your plastic surgeon and breast surgeon (surgical oncologist) is important. This is done by our office after your consultation.
Tell your surgeon about any medical problems you have, and any problems you may have had with surgery in the past. Most importantly, tell your doctor if you have had any hernias or any abdominal surgery in the past. Inform him what medications you take. These include prescription, non-prescription, herbs and supplements. You will be told which medications to stop and which to take before surgery. Aspirin and anti-inflammatory medications such as ibuprofen and Aleve must be stopped for 7 days before surgery. If you get sick or have any health issues in the days before surgery, please notify the office at once in case we have to postpone your operation.
The surgery and the incisions
Breast reconstruction can be performed immediately following a mastectomy (at the same surgery), or in a delayed fashion (from days to years later). Therefore, no matter how long ago your mastectomy was done you can still undergo breast reconstruction. Implant/expander reconstruction uses the same incisions as those used for the mastectomy. No new incisions are required. The TRAM and DIEP flaps harvest tissue from the abdomen and use the same incisions as in a tummy-tuck. The latissimus flap uses an incision on the back that can mostly be hidden within the bra line.
The length of surgery is highly variable. In addition to the time it takes the breast surgeon to perform her part, the reconstruction can take anywhere from an hour (for an implant/expander reconstruction) to 10 hours (for a complicated microsurgical procedure involving both breasts). Your surgeon will have a better estimate of the length of the procedure after your initial consultation.
The anesthesia
All breast reconstruction techniques are performed under general anesthesia. The second stage of an implant/expander reconstruction (replacement of the expander with an implant) can be performed either under “twilight” anesthesia or general anesthesia. Twilight anesthesia consists of intravenous sedation and pain medication that keeps you relaxed and sleepy during the surgery. In addition, the surgeon uses local anesthesia to numb the breast. General anesthesia involves going completely to sleep with a breathing tube in your throat. There is a slightly higher risk of nausea and vomiting after general anesthesia, however both techniques are extremely safe. Your surgeon will discuss the anesthetic options with you before surgery.
How long do I have to stay in the hospital?
Implant/expander reconstruction patients usually stay in the hospital for 1-2 days. Women who receive autogenous reconstruction with a TRAM or DIEP flap stay for 4-7 days. Those who undergo a latissimus flap stay somewhere in the middle (2-4 days).
How much pain is there after surgery?
Pain from breast reconstruction surgery is highly variable, and ranges from minimal to severe. Generally, implant reconstructions are less painful than autogenous reconstructions. The pain is worst in the first few days after surgery, but then it rapidly improves. It is impossible to predict a person’s expected pain. If you have done well with surgery in the past, you will likely be fine after this surgery. Our surgeons have a lot of experience treating pain, and have published scientific articles and written book chapters about anesthetics and pain control. They will do everything possible to minimize your pain, including using pain pumps after surgery and utilizing all the newest pain medication. By the end of the first week, most people’s pain is controlled with plain Tylenol or Motrin.
What about swelling and bruising?
Swelling and bruising are normal signs of the healing process. They occur after any surgery to varying degrees. Swelling peaks at about 48 hours, and then rapidly decreases. By the end of the first few weeks, 50 percent of the swelling is gone. By 6-8 weeks, a majority of the swelling has diminished. By six months, almost all the swelling is gone. Any remaining swelling is almost not perceptible. Bruising is worst the day after surgery and then rapidly gets better. It is usually gone by two weeks.
What restrictions are there after a TRAM or DIEP flap?
You can shower the day after surgery but you should not take a bath, use a hot-tub, or go swimming for at least two weeks. The first two days after surgery are usually spent lying in bed or sitting in a chair. Most patients then begin walking around the hospital hallways. Climbing stairs is difficult in the first few days after surgery, but becomes more manageable by the time of discharge. By the end of the first week, you will probably be ready for short trips and light walks. More vigorous walking and mild stretching exercises can be resumed about two weeks after surgery. Strenuous activities such jogging, aerobics, weight-training, sit-ups, and sex should not be done until 6 weeks after surgery. Also, you shouldn’t do any heavy lifting (over 10 pounds) during these 6 weeks.
What restrictions are there after an implant/expander reconstruction?
In general, implant reconstructions have fewer restrictions than autogenous reconstructions, and the postoperative recovery is much easier. Since all of the surgery is in the breasts, there is no difficulty with walking or moving around. After about two weeks, there are almost no lifting restrictions.
What kind of dressings and drains are there?
You can remove the gauze dressings the day after surgery. It is normal for a small amount of fluid to leak from the incisions for the first few days. This fluid looks like “Cool-aid” or fruit-punch and is part of the normal healing process. If you have leaking fluid that persists more than 48 hours after surgery, call the office. If there is tape or adhesive strips directly on your incision, do not remove these. If they fall off in the shower there is no need for concern.
Breast reconstruction requires that you have several drains after surgery. These help drain the fluid that is produced under your skin as part of the healing process. Without drains, this fluid can accumulate, termed a seroma. In some cases, a single drain may be sufficient, and in rare instances no drains are needed at all. They stay in until the drainage is less than 25 ml per drain in a twenty four hour period. This usually takes 5-7 days, but can be shorter or longer in some cases. The drains are easy to take care of, and do not hurt to take out.
When can I travel?
Traveling after surgery (air travel, long distance car trips, train rides, etc) should not be done before the drains are removed and you have had your first postoperative visit. Typically, this occurs 5-7 days after surgery. Patients who are at high risk for developing a blood clot should not travel until instructed by their surgeon. Short car trips under 60 minutes can be done before the first visit. A good rule of thumb is when you are off the stronger pain medication and can get up without assistance you are ready to go for a short drive. You should not drive the car yourself, however, until your surgeon gives you clearance for this.
When can I go back to work?
This, of course, depends on the kind of work you do. Most people go back to work after several weeks. Sedentary jobs, such as computer work or talking on the phone can begin even sooner. If you have a strenuous job that involves a lot of lifting or physical activity, you may have to wait 6 weeks until you are ready for work. Please review the restrictions for further guidelines about getting back to work.
What kind of scars can I expect?
Scarring is an unpredictable part of any surgery. It is impossible to cut through the full thickness of the skin and not have a scar. Our surgeons have published numerous scientific papers about the scarring process and wound healing, and will do everything possible to minimize scarring. To a large extent, however, scarring is determined by your genetics. If you are prone to hypertrophic (wide, raised) scars or keloids, make sure to inform your surgeon ahead of time. Our surgeons will use all the available techniques to minimize your scars based on their extensive research experience on hypertrophic scarring.
Your scars will be firm and pink for at least six weeks. After six weeks, scars are very strong and can withstand any activity. Then they may remain the same size for several months, or even appear to widen. After several months, your scars will begin to fade, although they will never disappear completely. It takes 1-2 years for a scar to completely heal. Make sure to apply sunscreen containing zinc-oxide to your scars for six months so that they do not darken due to increased pigmentation.
What if I have a problem? When should I call the office?
The Kryger Institute welcomes calls from patients. If you have any concerns at any time, please feel free to call our office. If it is an emergency, the answering service is available 24 hours a day including weekends and holidays. There is always a plastic surgeon on call. Your surgeon will discuss all the risks and potential complications with you before surgery. You will receive detailed instructions about situations that warrant a call to the office.
Post Mastectomy Lymphedema
Post mastectomy lymphedema is the abnormal swelling of the arm after undergoing a mastectomy or lymph node removal. The lymphatics in the armpit can get damaged after these surgeries resulting in swelling of the affected arm. This can lead to stiffness, pain and skin changes, in addition to an obvious difference in the size of the two arms.
Who gets it?
Any woman undergoing a mastectomy is at risk for lymphedema, but the risk is very low. In the range if 1-5%. The procedure with the greatest risk of developing lymphedema is when lymph nodes are removed from the armpit as part the of the cancer treatment, termed an axillary lymph node dissection. The risk of lymphedema from this procedure is as high as 20%. The addition of post surgical radiation therapy can increase this risk even higher.
What causes it?
Lymphedema can occur after surgery, when the lymphatic channels are cut in the process of removing lymph nodes. These channels normally connect to larger lymphatics that then drain from the armpit into the major veins that return all the blood to the heart. When the lymphatics are not draining properly, fluid backs up in the arm causing swelling.
How long does it last?
Lymphedema after breast cancer treatment can last from several months to many years. Unfortunately, without treatment it is usually permanent.
How do I know if I have it?
If you suspect that you may have post mastectomy lymphedema, you should see your surgical oncologist, or breast surgeon. He or she will take measurement of your arm and possibly order an imaging study such as a CT scan. In general, the diagnosis is made by the patient herself, who notices swelling of the arm and hand after surgery that does not get better.
What is the treatment of post mastectomy lymphedema?
Treatment begins with conservative measures such as a compression sleeve worn at all times, lymphatic massage to help restore flow of the fluids back to the heart, and specialized physical therapy. Severe cases may require surgery. Surgery is reserved for failure of conservative treatment
Surgical Treatment of lymphedema
Surgery is reserved for those cases that do not respond to conservative treatments. It involves repairing lymphatic channels in the armpit area, or connecting the severed lymphatics to small veins in the armpit that will then drain the lymphatic fluid back into the blood stream. It is a relatively minor procedure that can often be done as outpatient. Success rates vary and depend on many factors, such as the duration of lymphedema, the severity and the ability of the surgeon to locate functioning lymphatic channels. This delicate surgery is done by plastic surgeons, such as Drs. Kryger, with microsurgical training and the aid of a special surgical microscope.
Prevention of lymphedema
In patients undergoing an axillary lymph node dissection, the procedure that is at the highest risk of developing lymphedema, prophylactic surgery should be considered. Performing a lymphatic-venous anastomosis (connecting the cut lymphatics to small vein branches) at the time of the lymph node surgery has been shown to decrease the rate of lymphedema to below 5%. Ask your breast surgeon if this option is right for you.